Who We Are
Founded as a night school by Russell Conwell in 1884, Temple University has evolved into an international powerhouse in higher education and a top research institution with over 30,000 undergraduate, graduate and professional students. Today, led by President John A. Fry, our mission remains the same: we prioritize an accessible education and innovation in higher education, groundbreaking research, and celebrating our vibrant community of students, faculty and staff.
Philadelphia’s public university, Temple provides an unparalleled value and serves as an essential resource to the surrounding community.
We are committed to the ideals upon which Temple was founded.
- Providing access to an excellent, affordable higher education that prepares students for careers, further learning and active citizenship.
- Creating a collaborative community of outstanding faculty and staff who foster inclusion and encourage the aspirations of Temple students.
- Promoting service and engagement throughout Philadelphia, the commonwealth of Pennsylvania, the nation and the world.
What Sets Us Apart
Learn about just a few things that make Temple the home of limitless potential and endless opportunity by clicking and dragging through the tabs below.
Temple offers students a dynamic and nurturing learning environment with the support of a renowned faculty, dedicated academic advisors focused on setting a clear path to graduation and a broad curriculum of more than 600 academic programs. A longtime leader in professional education, Temple is also among the nation’s largest educators in the combined fields of dentistry, law, medicine, pharmacy and podiatry.
Temple also offers a gateway to the world with long-standing international campuses in Tokyo and Rome and study abroad opportunities across six continents.
Temple’s alumni are making an impact, one industry at a time. Temple has more than 370,000 graduates around the globe who stay connected and invested in the university and provide mentorship and professional development opportunities to aspiring changemakers in their respective fields.
Temple Athletics provides opportunities for its diverse student-athletes to unlock and maximize their potential, both in and out of the game. Whether you’re catching a basketball game at the Liacouas Center or a football game at Lincoln Financial Field, all of our athletic teams will make you proud to be a Temple Owl.
Temple’s bustling Main Campus is set against the backdrop of the Philadelphia skyline. Green space and eclectic architecture ranging from the historic Temple Performing Arts Center to the state-of-the-art Charles Library form a vibrant residential setting that our students and the surrounding community are proud to call home.
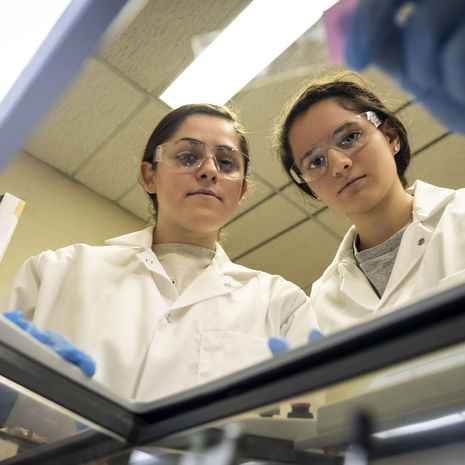
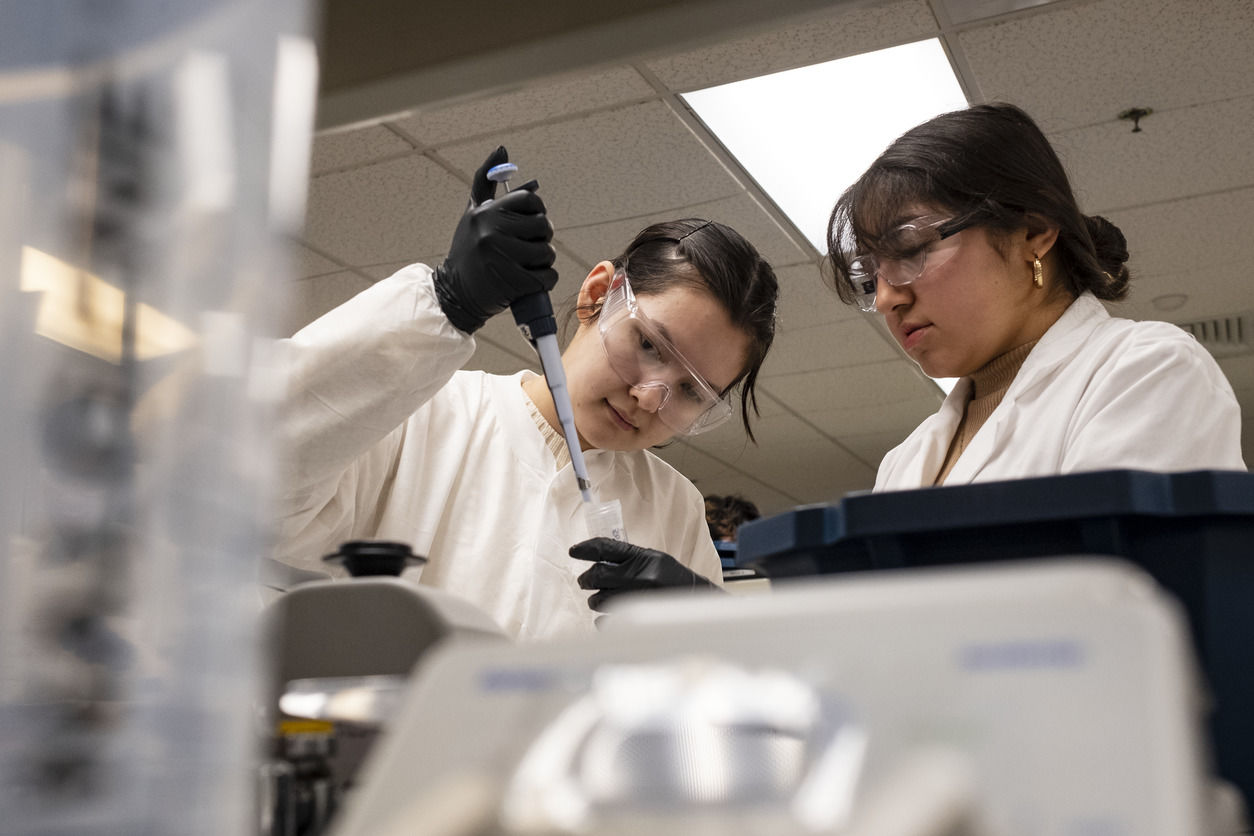
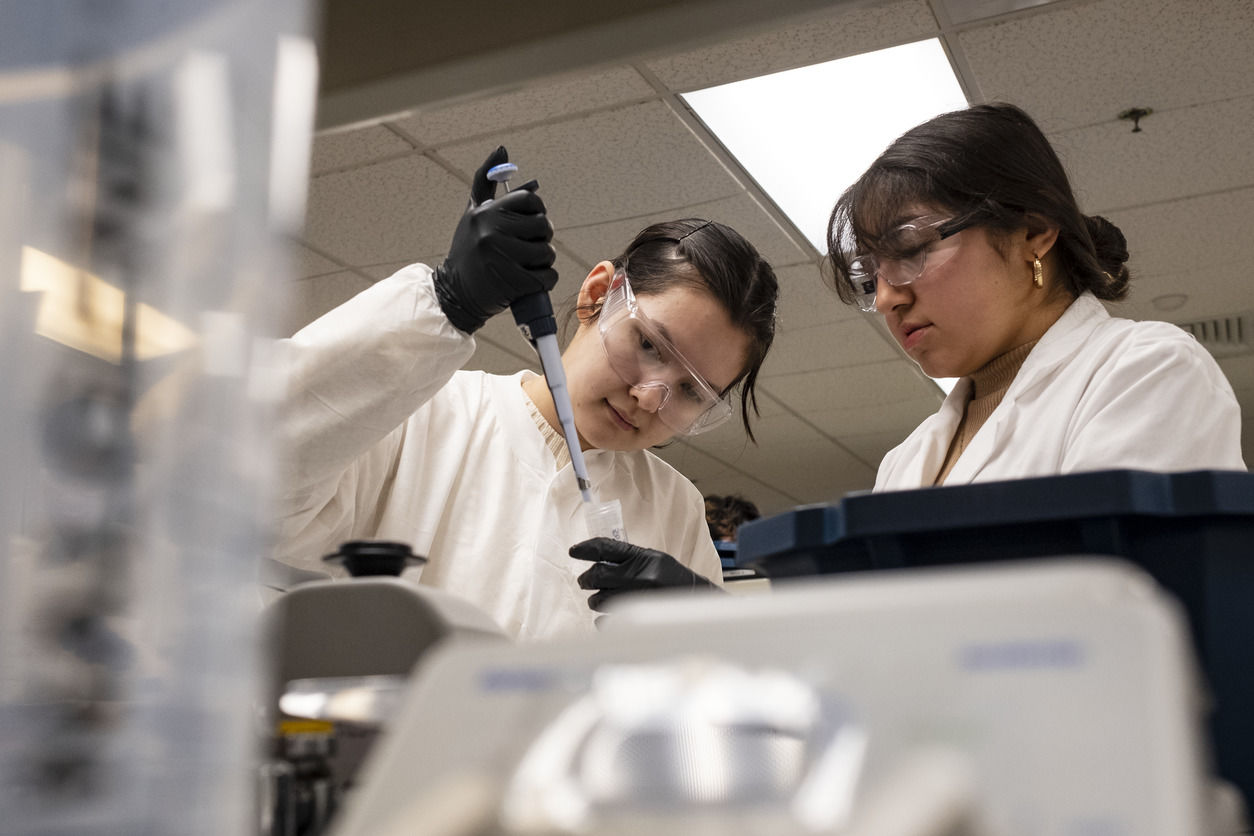
Learning and research facilities—from the Science, Education and Research Center and Sport Industry Research Center to our cutting-edge bioengineering labs and creative spaces at the Tyler School of Art and Architecture—enhance educational experiences and spark innovative ideas.
Our other campuses also house exceptional facilities, such as the Ambler Arboretum, that empower students to take their education to the next level.
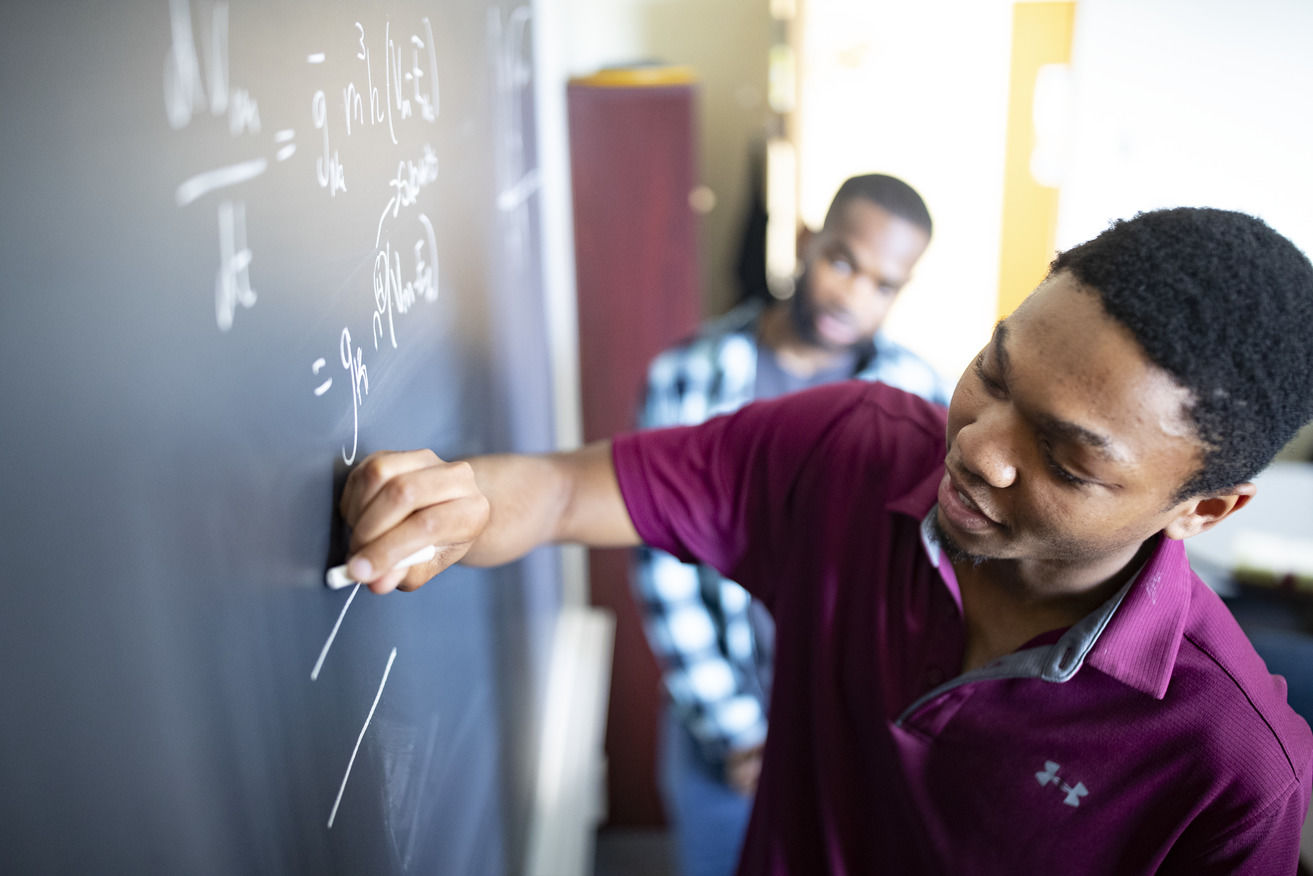
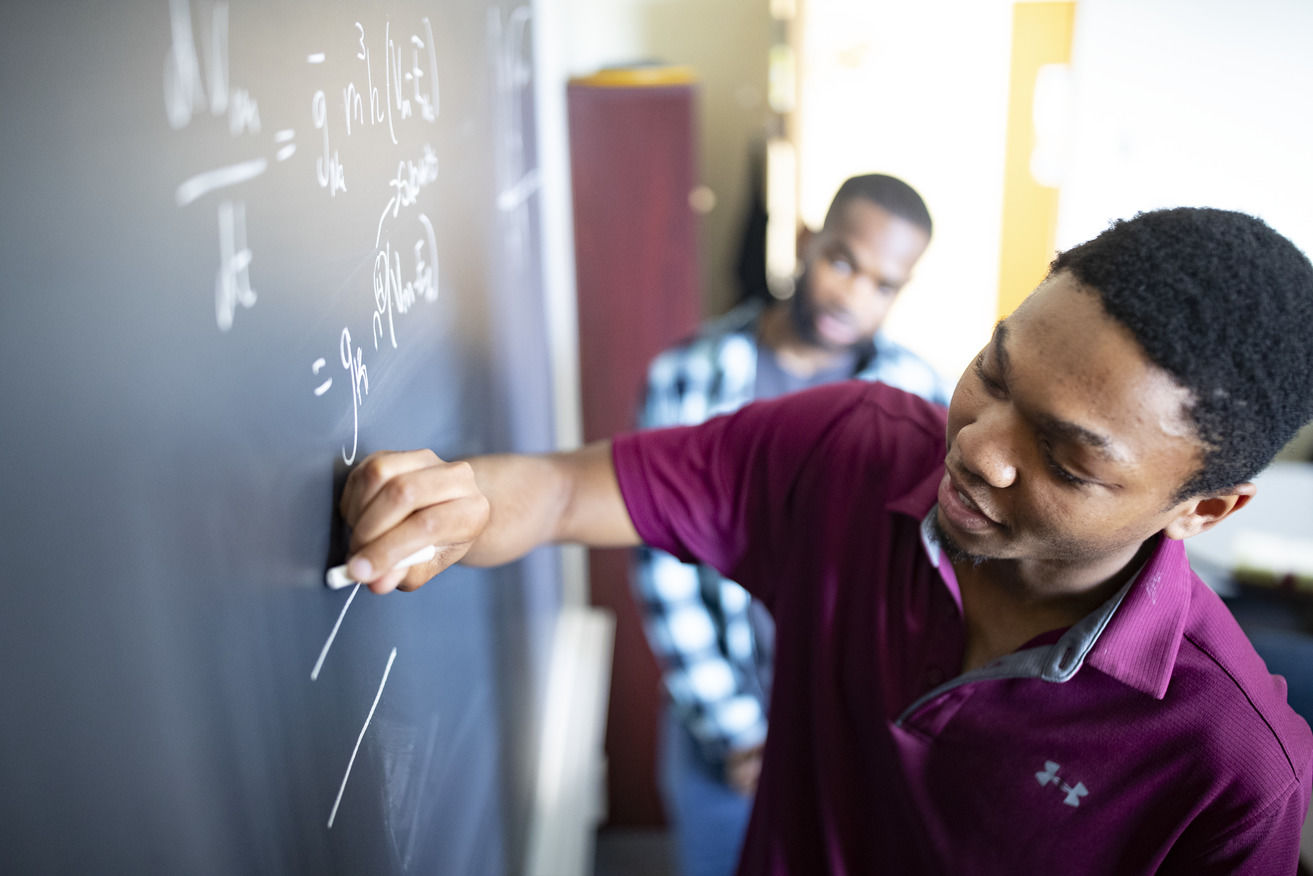
At Temple University, students learn from esteemed faculty members who bring a breadth of real-world experience, research achievements and a passion for their craft to the classroom. With a 12-1 student-faculty ratio, your professors do much more than just convey the subject material. You’ll be guided, mentored and encouraged as you join the next generation of Owls changing the world in your field.
Our faculty leverage Philadelphia to provide real-world experiences that enhance and enrich the academic experience. Students access the city for both the professional and social opportunities it affords. Whether you’re interning in Center City, immersing yourself in the city’s history in Old City, cheering on your favorite sports team at the Philadelphia Sports Complex or visiting an exhibit at the Philadelphia Museum of Art—your life at Temple extends far beyond the walls of campus.
Investments in the campus learning environment have elevated the university’s capabilities across its 17 schools and colleges with impressive results. And, students have opportunities to participate in the groundbreaking research that is conducted every day on campus. Temple is recognized as an R1 research institution by the Carnegie Classification of Institutions of Higher Education. The classification is given out only to institutions that demonstrate the “very high research spending and doctorate production."
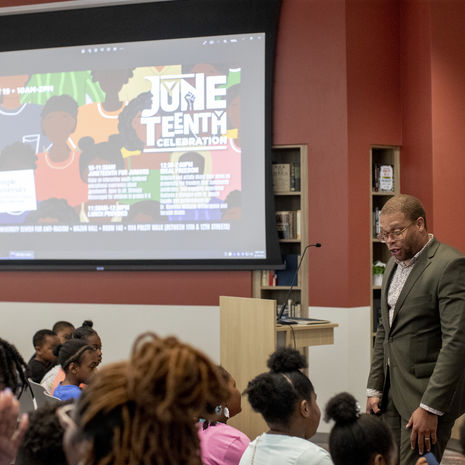
At Temple University, our 33,000+ students come together with a shared mission: to become the best versions of themselves. Your life at Temple University goes beyond attending classes. Whether you immerse yourself in arts and culture, athletic activities, community service opportunities, or student-run clubs, you’ll make lasting friendships and memories that will shape your future.
 View slideshow as list
View slideshow as list
















Who We Serve
Temple Health is a major Philadelphia-based academic health system that is driving medical advances through clinical innovation, pioneering research and world-class education. The health system’s 1,550+ physicians and scientists share a common mission of bringing tomorrow’s treatments to the bedside today, helping them achieve outcomes once thought impossible.
Read more about the doctors, researchers and other medical professionals who are making groundbreaking discoveries and advancing our community.